Nutritional advice for patients with advanced liver disease
Malnutrition and Liver Disease
Eating well is important to help prevent malnutrition and weight loss. Liver disease can result in a poor appetite, and an inability to absorb, store and process nutrients. Good nutrition can also assist in managing some complications of liver disease.
Malnutrition is very common in liver disease. Symptoms of poor appetite, feeling full quickly (due to ascites), weakness and fatigue, can make it difficult to meet increased protein and energy requirements. Loss of muscle mass and body fat stores are common as disease progresses. The body uses energy from the breakdown of muscles to survive. However despite being malnourished, body weight may appear normal due to excess fluid build up in the abdomen (ascites).
What should I eat?
Eating well is important to help prevent malnutrition and weight loss. Liver disease can result in a poor appetite, and an inability to absorb, store and process nutrients. Good nutrition can also assist in managing some complications of liver disease.
Malnutrition is very common in liver disease. Symptoms of poor appetite, feeling full quickly (due to ascites), weakness and fatigue, can make it difficult to meet increased protein and energy requirements. Loss of muscle mass and body fat stores are common as disease progresses. The body uses energy from the breakdown of muscles to survive. However despite being malnourished, body weight may appear normal due to excess fluid build up in the abdomen (ascites).
What should I eat?
- Try and eat small, frequent meals throughout the day. Eat 6 small meals, or eat every 2-4 hours during the day. This can help to prevent loss of muscle.
- Make sure each meal contains protein. Foods that are high in protein include meat, fish, poultry, dairy products (milk, cheese and yoghurt), eggs, nuts, seeds and legumes/pulses.
- To prevent protein/muscle breakdown and maintain blood sugar levels overnight, eat a protein rich and carbohydrate containing snack before going to bed. Examples include a sandwich, milkshake, fruit and yoghurt, or baked beans.
- Reduce the length of time without food overnight to less than 7 hours; have a nourishing drink or snack if you wake up in the middle of the night.
- Keep your diet low in salt. A diet high in salt can make ascites worse. Refer to salt section for more detail.
- If you have ascites, you may need to restrict the amount of fluid you drink.
- If your appetite is poor or you are unable to eat well, you may need to include a nutritional supplement to ensure that you consume adequate amounts of energy, protein and other nutrients. There are commercial supplements available which will be discussed later in this booklet. Your dietitian can provide you with more information about suitable supplements.
Protein
A high protein diet is important for people with chronic liver disease. Protein is used to maintain muscles and body tissues (including the liver) and to keep the body working normally.
Protein rich foods:
What are Nutritional Supplements?
Nutritional supplements are special food products or powders that can be used as part of, or in addition to, your daily food intake. They add extra energy, protein, and vitamins and minerals.
Supplements are helpful for people who:
The amount of supplement you require will depend on your food intake. If your food intake decreases, you will need more supplements. Discuss with your dietitian the type of supplement and the amount you need.
Nutrition supplements are available in snack bars, powders, ready-to-drink varieties, and puddings. They can be purchased from the supermarket (selected products only), chemists, and through the hospitals’ Home Enteral Nutrition (HEN) Service. Your dietitian will need to register you with the HEN service.
Energy Powders (e.g. Polyjouleä) and Protein Powders (e.g. Beneproteinä) can be added directly to drinks and food without altering the taste.
A specialised protein supplement containing branched chain amino acids may be prescribed for patients with hepatic encephalopathy to minimise symptoms and prevent further breakdown of muscles. Discuss this with your dietitian.
A high protein diet is important for people with chronic liver disease. Protein is used to maintain muscles and body tissues (including the liver) and to keep the body working normally.
Protein rich foods:
- Meat, chicken, fish and seafood
- Eggs
- Milk, yoghurt, cheese, custard, ice cream
- Legumes (lentils, split peas, soy beans, baked beans etc)
- Nuts and seeds
What are Nutritional Supplements?
Nutritional supplements are special food products or powders that can be used as part of, or in addition to, your daily food intake. They add extra energy, protein, and vitamins and minerals.
Supplements are helpful for people who:
- Have lost weight
- Have difficulty in maintaining their weight
- Have a poor appetite
- Are not eating enough food
The amount of supplement you require will depend on your food intake. If your food intake decreases, you will need more supplements. Discuss with your dietitian the type of supplement and the amount you need.
Nutrition supplements are available in snack bars, powders, ready-to-drink varieties, and puddings. They can be purchased from the supermarket (selected products only), chemists, and through the hospitals’ Home Enteral Nutrition (HEN) Service. Your dietitian will need to register you with the HEN service.
Energy Powders (e.g. Polyjouleä) and Protein Powders (e.g. Beneproteinä) can be added directly to drinks and food without altering the taste.
A specialised protein supplement containing branched chain amino acids may be prescribed for patients with hepatic encephalopathy to minimise symptoms and prevent further breakdown of muscles. Discuss this with your dietitian.
Fluid Restriction
If you have ascites, your doctor may recommend a fluid restriction, usually between 1200mL and 1500mL per day. This is to help reduce the build up of excess fluid in the abdominal cavity. Ascites will make you gain weight due to the weight of fluid. Sometimes this fluid needs to be drained by your doctor.
Focus on drinking nourishing fluids such as milk based drinks, or nutrition supplements will provide you with additional energy and/or protein. Try not to fill up on tea, coffee, water or diet/low joule drinks as these do not provide any protein or energy.
These hints may assist you in monitoring your fluid intake:
If you have ascites, your doctor may recommend a fluid restriction, usually between 1200mL and 1500mL per day. This is to help reduce the build up of excess fluid in the abdominal cavity. Ascites will make you gain weight due to the weight of fluid. Sometimes this fluid needs to be drained by your doctor.
Focus on drinking nourishing fluids such as milk based drinks, or nutrition supplements will provide you with additional energy and/or protein. Try not to fill up on tea, coffee, water or diet/low joule drinks as these do not provide any protein or energy.
These hints may assist you in monitoring your fluid intake:
- Spread your fluid intake out over the day and only drink when you are thirsty.
- Measure the volume of your favourite cup/mug so you can keep track of the amount of fluid you drink each day.
- Serve yourself ‘half cups’ rather than a full cup of fluid
- Eat less salty foods. By limiting the amount of salty foods you eat, you will be less thirsty.
Salt Restriction in Liver Disease
Salt is also known as sodium. Some salt is found in all the foods we eat. We often eat more salt than we need. A high salt diet can cause the body to retain extra fluid making your ascites worse.
Your doctor may recommend a 2g per day (or 2000mg) salt restriction to help prevent the recurrence of ascites.
The following suggestions can help you to reduce your salt intake:
- Do not add salt during cooking or at the table
- Avoid processed/high salt foods (such as luncheon meats, crisps)
- Select no added salt, low salt, low sodium or salt reduced products
- Use herbs and spices to add extra flavour to your food
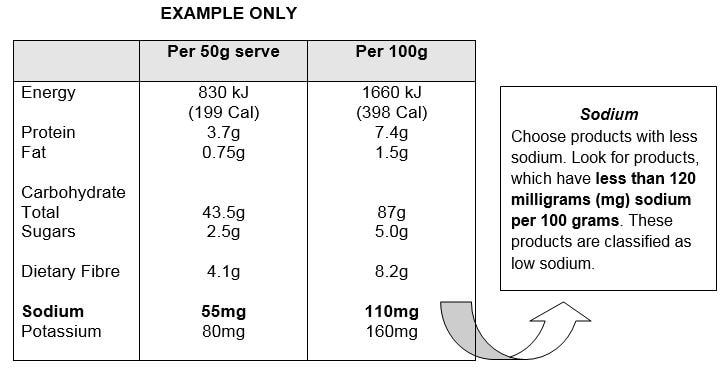
Label reading for salt
Low salt and low sodium foods are defined as having a sodium content of 120mg/100g or less. However, very few foods available in the supermarket have a sodium content this low. For a reduced salt diet, it is generally accepted to have a sodium content of 300-400mg/100g. The nutrition information panel will list the actual amount of salt in the product.
This product would be considered low sodium and so is a good choice.
Remember sodium is found in rock salt, sea salt, table salt, mineral salt, chicken salt and vegetable salt. If you are struggling to eat enough, your doctor or dietitian may relax your salt restriction for a time.
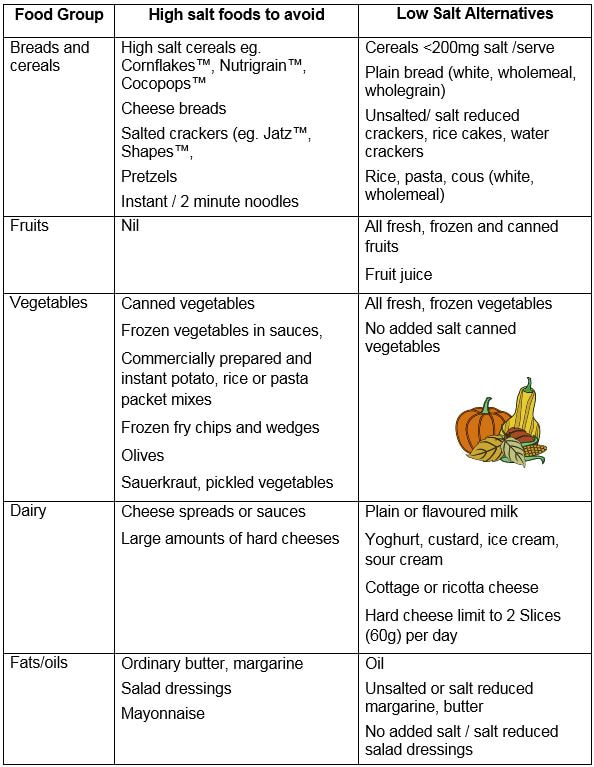
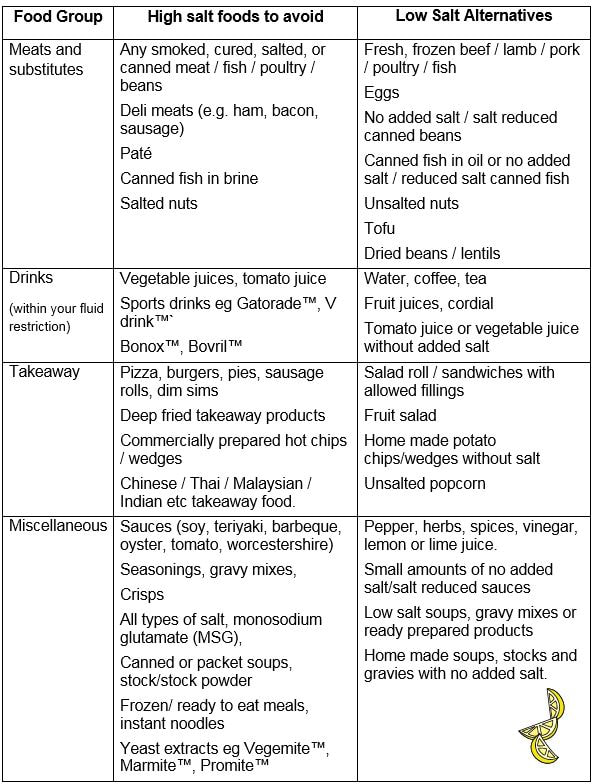
The table on below is a list of high salt foods to avoid in order to limit your salt intake.
The mention of product names in this resource does not constitute endorsement by dietitians of WSLHD.
This information is provided with individualised advice by an Accredited Practicing Dietitian.
This information is provided with individualised advice by an Accredited Practicing Dietitian.
Developed by Department of Nutrition and Dietetics Westmead Hospital, Western Sydney LHD, April 2012. Reviewed March 2018
Contact Us
[email protected]
[email protected]